If I had a previous stroke or transient ischemic attack (TIA) how likely will I have stroke again?
Blog post description.
8/27/20253 min read
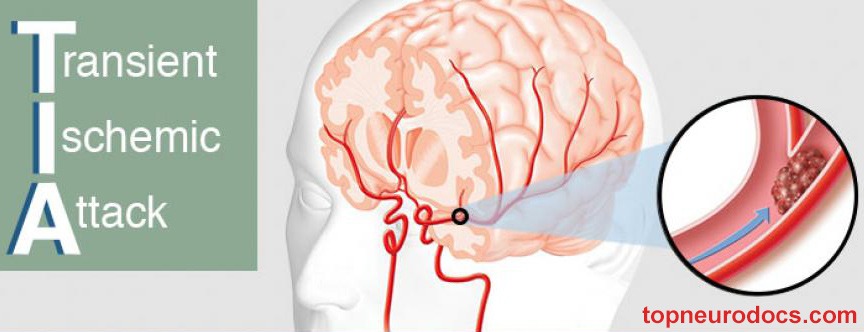

If I had a previous stroke or transient ischemic attack (TIA) how likely will I have stroke again?
Having had a stroke or a transient ischemic attack (TIA) in the past does increase the risk of having another stroke compared to someone who has never had one. Here are some key points from medical research and guidelines:
Risk after TIA: About 1 in 5 people who have a TIA will go on to have a stroke within 90 days, and the risk is highest in the first few days.
Risk after stroke: After a first stroke, the chance of a recurrent stroke is roughly 5–15% within the first year, and then about 2–4% per year thereafter, depending on risk factors and treatment.
Risk factors: High blood pressure, diabetes, smoking, high cholesterol, atrial fibrillation, and not taking prescribed medications (such as blood thinners or antiplatelets) all significantly increase recurrence risk.
Prevention: With proper treatment—blood pressure control, cholesterol management, lifestyle changes, and sometimes blood thinners or antiplatelet therapy—the risk of recurrence can be cut substantially.
👉 The most important step is to work closely with your healthcare provider to manage your personal risk factors and follow the prevention plan prescribed for you.
Here are some of the common strategies doctors often recommend after a TIA or stroke to reduce the chance of another one (these are general guidelines, not a substitute for medical advice):
1. Medications (as prescribed by a doctor):
Antiplatelet drugs (like aspirin or clopidogrel) or anticoagulants (like warfarin or newer agents if you have atrial fibrillation).
Blood pressure medications to keep blood pressure well controlled.
Cholesterol-lowering drugs (statins) even if cholesterol is not very high.
Diabetes medications if needed for blood sugar control.
2. Lifestyle changes:
Quit smoking if you smoke.
Eat a heart-healthy diet (plenty of fruits, vegetables, whole grains, lean proteins, and less salt and processed foods).
Exercise regularly — usually at least 150 minutes of moderate activity per week, if your doctor says it is safe.
Maintain a healthy weight.
Limit alcohol (generally no more than 1 drink/day for women, 2 for men, or less if advised).
3. Medical follow-up:
Regular check-ups with your healthcare provider.
Monitoring for atrial fibrillation or other heart rhythm problems.
Keeping track of blood pressure at home if recommended.
4. Other considerations:
Manage sleep apnea if present.
Reduce stress and prioritize good sleep.
Participate in a stroke rehabilitation program if you still have lingering effects.
⚠️ Since everyone’s situation is different, it is really important to follow the exact plan your doctor prescribes.
A simple way to remember the major warning signs of stroke is the acronym F.A.S.T.:
F – Face: Sudden drooping or numbness on one side of the face. Ask the person to smile — does one side droop?
A – Arm: Sudden weakness or numbness in one arm. Ask the person to raise both arms — does one drift downward?
S – Speech: Sudden trouble speaking, slurred speech, or difficulty understanding others.
T – Time: If you see any of these signs, it is time to call emergency services right away (e.g., 911 in the U.S.).
Other possible warning signs can include:
Sudden vision loss or blurriness in one or both eyes.
Sudden dizziness, loss of balance, or difficulty walking.
Sudden severe headache with no known cause.
⚠️ Stroke is a medical emergency. Even if symptoms go away quickly (like in a TIA), you should seek immediate medical attention — early treatment can save brain tissue and prevent long-term disability.
What usually happens when someone comes to the hospital with possible stroke symptoms.
Here is a general overview (it can vary depending on the hospital and the person’s condition):
1. Immediate triage and assessment
Stroke is treated as an emergency — patients are taken quickly to a special area (often a “stroke team” is activated).
Vital signs (blood pressure, heart rate, oxygen) are checked right away.
A focused neurological exam is done to assess strength, speech, vision, and alertness.
2. Rapid brain imaging
A CT scan (or sometimes MRI) of the brain is done urgently to see whether the stroke is caused by a blood clot (ischemic stroke) or bleeding (hemorrhagic stroke). This distinction is critical because treatments differ.
3. Blood tests and monitoring
Blood sugar, clotting factors, and other labs are checked.
Heart monitoring (ECG) is done to look for atrial fibrillation or other rhythm problems.
4. Emergency treatment (if eligible and within time window)
Ischemic stroke (blocked artery):
Intravenous clot-busting medication (tPA/alteplase) may be given if within a certain time window (usually up to 4.5 hours from symptom onset).
In some cases, a mechanical thrombectomy (a catheter procedure to remove the clot) may be performed, especially if a large artery is blocked and it is within up to 6–24 hours.
Hemorrhagic stroke (bleeding):
Focus is on controlling blood pressure, stopping any blood-thinning medications, and sometimes surgery to relieve pressure or repair a ruptured vessel.
5. Hospital care and prevention of complications
Patients are admitted to a stroke unit or intensive care for close monitoring.
Swallowing ability is checked to reduce risk of aspiration pneumonia.
Physical, occupational, and speech therapy may begin very early.
Doctors also start planning for secondary prevention (blood pressure control, cholesterol medications, antiplatelet/anticoagulants, lifestyle changes).
⚠️ If you or someone else ever develops sudden stroke symptoms, the most important thing is to call emergency services immediately. Time lost is brain lost.