If you have High cholesterol, are you at risk of having a stroke?
Blog post description.
8/27/20258 min read
If you have High cholesterol, are you at risk of having a stroke?
Yes, having high cholesterol does increase your risk of having a stroke. Here is why:
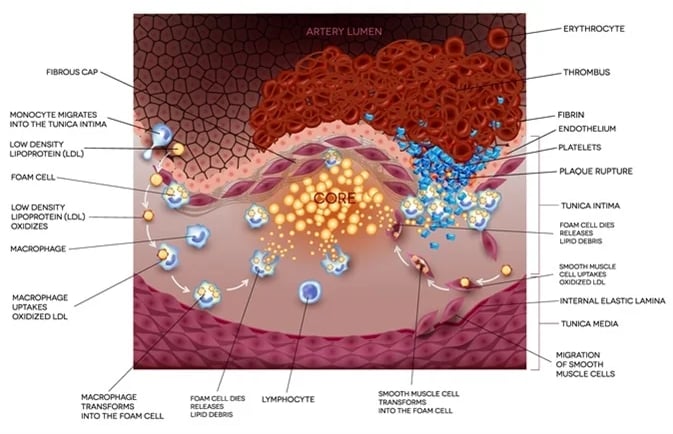
Cholesterol and plaque buildup: When cholesterol levels are high—especially LDL ("bad" cholesterol)—it can lead to fatty deposits (plaques) forming inside your arteries.
Narrowing and hardening of arteries: These plaques can narrow or harden the arteries (atherosclerosis), reducing blood flow to the brain.
Blockages or clots: If a plaque ruptures, it can cause a blood clot to form. If that clot blocks blood flow to the brain, it can result in an ischemic stroke (the most common type).
Additional risk factors: High cholesterol often goes hand-in-hand with other stroke risk factors, such as high blood pressure, diabetes, smoking, and obesity.
The good news: High cholesterol is a modifiable risk factor. Lifestyle changes (healthy diet, exercise, quitting smoking, limiting alcohol) and, if needed, medications (like statins) can significantly lower your risk of stroke and heart disease.
Here are some practical, evidence-based steps you can take to lower cholesterol and reduce your risk of stroke:
1. Improve your diet
Eat more fiber: Foods like oats, beans, lentils, fruits, and vegetables help lower LDL (“bad”) cholesterol.
Choose healthy fats: Use olive oil, nuts, seeds, and fatty fish (like salmon or mackerel) instead of butter, lard, or processed oils.
Limit trans fats and saturated fats: Found in fried foods, processed snacks, red meat, and full-fat dairy.
Increase plant-based foods: More vegetables, fruits, and whole grains support heart and vascular health.
2. Stay physically active
Aim for at least 150 minutes of moderate exercise per week (like brisk walking, cycling, or swimming).
Physical activity helps raise HDL (“good”) cholesterol and lower LDL.
3. Maintain a healthy weight
Even modest weight loss (5–10% of body weight) can improve cholesterol levels and reduce stroke risk.
4. Quit smoking
Smoking damages blood vessels, lowers good cholesterol, and makes clots more likely.
5. Limit alcohol
If you drink, do so in moderation (up to 1 drink/day for women, up to 2 for men). Excess alcohol can raise cholesterol and blood pressure.
6. Manage other health conditions
Keep blood pressure and blood sugar under control if you have hypertension or diabetes.
7. Consider medications if needed
If lifestyle changes are not enough, your doctor may prescribe statins or other cholesterol-lowering medications.
⚠️ It is important to work with your healthcare provider to check your cholesterol levels and overall risk factors, and to decide on the best plan for you.
Knowing the warning signs of a stroke is very important, because getting help quickly can save brain function and even save a life.
A simple way to remember the key signs is the acronym FAST:
F – Face drooping: One side of the face may droop or feel numb. Ask the person to smile — is it uneven?
A – Arm weakness: One arm may drift downward when both arms are raised.
S – Speech difficulty: Speech may be slurred, hard to understand, or the person may not be able to speak at all.
T – Time to call emergency services: If you see any of these signs, call emergency services right away (e.g., 911 in the U.S.).
Other possible stroke symptoms include:
Sudden numbness or weakness in the leg, especially on one side of the body
Sudden confusion or trouble understanding speech
Sudden trouble seeing in one or both eyes
Sudden trouble walking, dizziness, loss of balance or coordination
Sudden severe headache with no known cause
⚠️ Stroke is a medical emergency — the sooner treatment begins, the better the chances of recovery.
Understanding the difference difference between a stroke and a mini-stroke (TIA)? can help you know when to get urgent care.
Stroke vs. TIA (Transient Ischemic Attack)
Stroke:
Happens when blood flow to part of the brain is blocked (ischemic stroke) or when a blood vessel bursts (hemorrhagic stroke).
Causes brain cells to start dying within minutes.
Symptoms often last longer than 24 hours and may cause permanent damage.
TIA (mini-stroke):
Caused by a temporary blockage of blood flow to the brain.
Symptoms are the same as a stroke, but they usually last only a few minutes to a couple of hours and resolve completely within 24 hours.
A TIA does not cause permanent brain damage, but it is a serious warning sign. Having a TIA means you are at much higher risk of having a full stroke in the near future.
👉 Key point: Even if symptoms go away quickly, a TIA is an emergency — you should still seek medical care immediately. Doctors can investigate the cause and start treatment to prevent a major stroke.
Here is an overview of the main tests’ doctors may use if they suspect a stroke or TIA:
1. Brain Imaging
CT scan (Computed Tomography):
Usually, the first test done.
Quickly shows if there’s bleeding in the brain (hemorrhagic stroke) or signs of an ischemic stroke.
MRI (Magnetic Resonance Imaging):
Provides more detailed images than a CT.
Can detect smaller strokes or TIAs that a CT might miss.
2. Blood Vessel Imaging
CT angiography or MR angiography: Looks at blood vessels in the brain and neck to check for blockages or narrowing.
Carotid ultrasound: Uses sound waves to see if the carotid arteries (in the neck) are narrowed or blocked.
3. Heart Tests
Electrocardiogram (ECG/EKG): Checks for heart rhythm problems (like atrial fibrillation) that can cause blood clots leading to stroke.
Echocardiogram: Uses ultrasound to see the heart’s structure and function, and to look for clots or other sources of emboli.
4. Blood Tests
Check for risk factors and complications, such as:
Cholesterol levels
Blood sugar (diabetes)
Clotting function
Infections or other underlying conditions
5. Neurological Exam
Doctors test reflexes, strength, coordination, vision, speech, and mental status to assess which part of the brain may be affected.
⚠️ If stroke is suspected, time is critical. Imaging is usually done immediately to decide the best treatment (like clot-busting drugs or procedures).
Treatment depends on whether it is a stroke (and what type) or a TIA. Here is an overview:
🧠 Stroke Treatments
1. Ischemic Stroke (caused by a clot blocking blood flow — most common type)
Clot-busting medication (tPA):
Given through a vein, ideally within 3–4.5 hours of symptom onset.
Helps dissolve the clot and restore blood flow.
Mechanical thrombectomy:
A procedure where doctors insert a catheter into a blood vessel to physically remove the clot.
Usually performed within 6–24 hours of symptom onset, depending on the case.
Blood thinners / antiplatelet drugs:
Medications like aspirin or other agents may be given to reduce the risk of new clots.
2. Hemorrhagic Stroke (caused by bleeding in the brain)
Emergency measures to control bleeding:
Medications to lower blood pressure, reduce brain swelling, or reverse blood thinners.
Surgery or procedures:
To repair blood vessels, remove blood, or relieve pressure inside the skull.
⚡ TIA (Transient Ischemic Attack)
Symptoms resolve on their own, but treatment is crucial to prevent a future stroke.
Doctors may prescribe:
Antiplatelet medications (like aspirin)
Blood thinners if caused by atrial fibrillation or another clotting problem
Cholesterol-lowering drugs (statins)
Blood pressure medications if hypertension is present
In some cases, surgery or stenting may be done to open narrowed carotid arteries.
🌱 Rehabilitation & Prevention
After a stroke (or TIA), treatment also focuses on:
Physical, occupational, and speech therapy to regain function.
Lifestyle changes: healthy diet, exercise, quitting smoking, limiting alcohol.
Managing risk factors: controlling cholesterol, diabetes, and blood pressure.
⚠️ Key point: Stroke is always a medical emergency — the sooner treatment starts, the better the chances of recovery and survival. A TIA is also a warning sign not to ignore.
A very important part of understanding stroke care, because recovery does not end after the emergency treatment. Long-term recovery can vary a lot depending on the type of stroke, the area of the brain affected, and how quickly treatment was given. Here is what to expect:
🕒 Phases of Recovery
1. Acute phase (hospital stay):
· Focus is on stabilizing the patient, preventing complications, and starting early rehab.
· Length of stay may be a few days to weeks.
2. Rehabilitation phase:
· Begins as soon as possible, often in a rehab unit or outpatient setting.
· Can last weeks to months, depending on needs.
3. Long-term recovery phase:
· Ongoing therapy and lifestyle adjustments.
· Some people recover fully, while others may have lasting challenges.
🏋️ Rehabilitation Therapies
Physical therapy: Helps regain strength, balance, and coordination.
Occupational therapy: Focuses on relearning daily activities (dressing, cooking, driving).
Speech and language therapy: For communication or swallowing difficulties.
Neuropsychological support: Addresses memory, problem-solving, and emotional changes.
💡 Possible Long-Term Effects
Physical: Weakness or paralysis on one side, balance issues, fatigue.
Cognitive: Memory problems, trouble concentrating, slower thinking.
Communication: Difficulty speaking, understanding, reading, or writing.
Emotional/behavioral: Depression, anxiety, mood swings, frustration.
🌱 Prevention & Lifestyle Changes
Control blood pressure, cholesterol, and blood sugar.
Take prescribed medications (antiplatelets, statins, blood thinners if needed).
Eat a heart-healthy diet (low in salt, saturated fats, and processed foods).
Exercise regularly (as approved by your doctor).
Quit smoking and limit alcohol.
🤝 Support Systems
Family and caregiver support is crucial.
Stroke support groups can help with emotional recovery.
Regular follow-ups with doctors to monitor risk factors and progress.
⚠️ Key takeaway: Recovery is often a marathon, not a sprint. Many people continue to improve for months or even years after a stroke, especially with consistent therapy and support.
Supporting someone after a stroke can be both rewarding and challenging. Here are some practical tips for caregivers:
🏠 Daily Care & Safety
Create a safe environment: Remove trip hazards, add grab bars in the bathroom, and ensure good lighting.
Encourage independence: Allow the person to do as much as they can safely, even if it takes longer — it helps rebuild confidence.
Establish routines: Consistency reduces stress and helps with memory and focus.
🏋️ Support Rehabilitation
Practice exercises at home: Reinforce what therapists teach (mobility, speech, or memory exercises).
Celebrate small progress: Recovery can be slow — encouragement makes a big difference.
Be patient: Tasks may take longer, and frustration is common.
💬 Communication Tips
If speech is affected:
Use simple sentences and yes/no questions.
Give extra time to respond.
Use gestures, pictures, or writing if needed.
💡 Emotional Support
Watch for depression or anxiety: These are common after stroke. Encourage open conversations and seek professional help if needed.
Stay positive but realistic: Acknowledge challenges while focusing on progress.
Encourage social interaction: Isolation can slow recovery.
🧑⚕️ Caregiver Self-Care
Take breaks: Caregiving can be exhausting — arrange respite care when possible.
Look after your health: Eat well, exercise, and get enough sleep.
Seek support: Join caregiver or stroke support groups for advice and emotional support.
📋 Medical Management
Track medications: Use pill organizers or reminders to prevent missed doses.
Monitor risk factors: Help with blood pressure checks, diet, and follow-up appointments.
Know the warning signs of another stroke: Remember FAST (Face, Arm, Speech, Time).
⚠️ Key point: Caregivers are partners in recovery, but they also need support themselves. Taking care of your own well-being helps you provide better care.
A sample daily routine. Of course, every stroke survivor’s needs and abilities are different, so this is just a general framework that can be adjusted based on medical advice, therapy schedules, and energy levels.
🗓️ Sample Daily Routine for Stroke Recovery
🌅 Morning
7:00 AM – Wake up & morning hygiene
Assistance with washing, dressing, and grooming if needed.
Encourage the person to do as much as possible independently.
7:30 AM – Breakfast & medications
Include heart-healthy foods (whole grains, fruit, lean protein).
Take prescribed medications with food/water.
8:30 AM – Light physical therapy/exercise
Gentle stretching, walking with support, or therapist-recommended exercises.
Helps improve circulation and mobility early in the day.
☀️ Midday
10:00 AM – Rest/quiet activity
Reading, listening to music, or light conversation.
Fatigue is common, so short breaks are important.
11:00 AM – Speech/occupational therapy practice
Work on speech exercises, memory tasks, or daily living skills (buttoning clothes, cooking practice).
12:30 PM – Lunch
Balanced meal with vegetables, lean protein, and whole grains.
Social time can help mood and communication.
🌤️ Afternoon
1:30 PM – Rest/nap
Short naps help manage fatigue without disrupting nighttime sleep.
2:30 PM – Physical activity/rehab exercises
More intensive therapy if energy allows, or a short walk.
3:30 PM – Leisure/social activity
Phone call with family, puzzle, card game, or supervised hobby.
Keeps the mind active and prevents isolation.
🌙 Evening
5:30 PM – Dinner & medications
Lighter meal with focus on vegetables and lean protein.
6:30 PM – Relaxation time
Watch TV, listen to music, or quiet conversation.
Gentle stretching or breathing exercises can help reduce stress.
8:00 PM – Caregiver check-in
Review the day’s progress, note any symptoms, and prepare for the next day.
9:00 PM – Bedtime routine
Hygiene, medications if prescribed, and a calm environment for sleep.
🤝 Caregiver Balance
Use rest periods to take breaks for yourself (walk, read, or connect with friends).
Share responsibilities with family or respite services when possible.
Keep a daily log of exercises, meals, medications, and mood to track progress and spot changes.
⚠️ Important: Always follow the rehab team’s personalized plan. This routine is just a template — therapy intensity, rest needs, and independence will vary.